Antibiotics and the sustainable production of food
- Like
- Digg
- Del
- Tumblr
- VKontakte
- Buffer
- Love This
- Odnoklassniki
- Meneame
- Blogger
- Amazon
- Yahoo Mail
- Gmail
- AOL
- Newsvine
- HackerNews
- Evernote
- MySpace
- Mail.ru
- Viadeo
- Line
- Comments
- Yummly
- SMS
- Viber
- Telegram
- Subscribe
- Skype
- Facebook Messenger
- Kakao
- LiveJournal
- Yammer
- Edgar
- Fintel
- Mix
- Instapaper
- Copy Link
Posted: 29 August 2017 | Dr Grace O’Gorman | Technical Policy Assistant | NOAH | No comments yet
Antibiotics are an essential resource for the health and welfare of people and animals. They also positively contribute to the growing global demand for safe and sustainable food from animals. At the same time there is growing concern about the developing human medical antimicrobial resistance (AMR) crisis, which has focused attention on antibiotic use in people and animals. In this article, NOAH’s Grace O’Gorman explains the implications for the food chain.
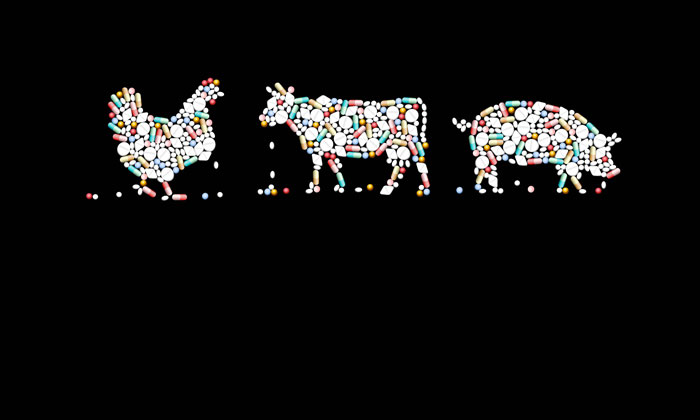
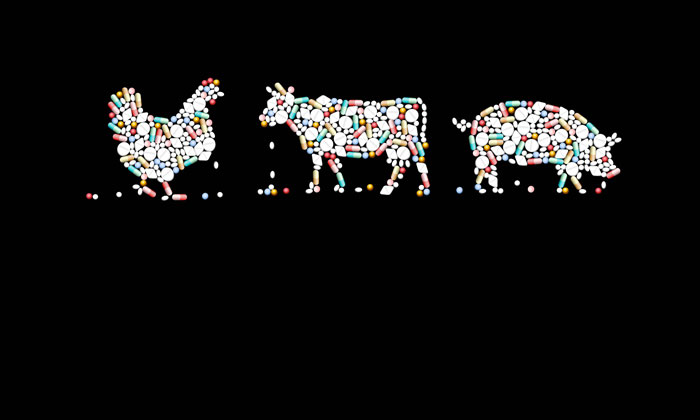
ALTHOUGH it is acknowledged that the clinical problems in human medicine are primarily due to antibiotic use in people, AMR is a significant One Health issue and antibiotics need to be used responsibly in both human and veterinary medicine to maintain their effectiveness as a crucial shared resource into the future1. The response to this challenge has gathered great momentum in recent years and builds on the safeguards already in place to sustainably produce safe food and protect consumers2.
Before an antibiotic can be used on a farm for the treatment of animals it must be assessed and approved for use by independent regulatory authorities.
The foundation of producing safe food on a farm begins with healthy animals. Vets and farmers work together to develop farm health plans that have a range of preventative health strategies at their core. Taking a holistic approach ensures that a range of measures are put in place to prevent or reduce disease burden, eg, use of vaccination, good biosecurity and hygiene. Nevertheless, despite these measures, animals will from time-to-time succumb to bacterial disease and may require antibiotics regardless of the farming system. Responsible use practices include prompt and appropriate treatment to minimise morbidity, mortality and the further spread of disease in flocks or herds. Animals that are unwell are also less productive and so there is an economic cost associated with disease that impacts the ability of farmers to sustainably produce food from animals.
Assessment
Before an antibiotic can be used on a farm for the treatment of animals it must be assessed and approved for use by independent regulatory authorities. Rigorous European and UK standards for the registration process ensure only those medicines that meet defined standards of quality, safety (including consumer safety for medicines used in food producing animals) and efficacy are authorised for use. All antibiotics for farm animals in the UK are legally classified as prescription-only medicines, which means they can only be prescribed by a veterinary surgeon who makes considered decisions about prescribing antibiotics under a professional code of conduct3. Based on clinical judgement, treatment may be prescribed to individual sick animals or groups of animals as appropriate. The dynamics of disease spread in groups of farm animals are such that those in contact with clinical cases are at high risk of disease or may already be sub-clinically infected. Decisions by the farm vet combine and balance responsibilities to protect the health and welfare of all animals under their care with public health. Best practice acknowledges that treatment for groups of animals should never occur on a routine ongoing basis or to compensate for poor husbandry practices4,5.
Consumer safeguards continue after antibiotics are prescribed for food-producing animals. All medicines used in animals are strictly controlled by the Veterinary Medicines Regulation in the UK and European law6,7. These include requirements for farmers to record all medicines bought and administered. The withdrawal period, which is the time that must elapse from the last dose until the animal is allowed to enter the food chain, must be recorded and observed for all medicines for food producing animals, including antibiotics. Despite the confusion on terminology and understanding of various ‘antibiotic-free’ food labels, the scientifically determined withdrawal period means that residues in food from treated animals will have depleted below the Maximum Residue Limit and food is safe to consume8. There is a legislative requirement for the Government to run a surveillance programme, analysing samples from food-producing animals for residues of veterinary medicines. Results are published by the Veterinary Medicines Directorate (VMD), which shows that the vast majority of samples are compliant9.
Task Force
For 20 years the Responsible Use of Medicines in Agriculture Alliance (RUMA) has co-ordinated a consistent approach and published guidelines on best practice in animal medicine use, including antibiotics. More recently, RUMA has accelerated efforts and formed a Targets Task Force, which is developing antibiotic responsible use objectives for each of the livestock sectors in the UK. This work will carefully consider and balance actions on AMR with the need to maintain good animal health and welfare standards10. In line with promoting consistency and an evidence-based approach, RUMA recently adopted the EMA AMEG opinion on the categorisation of Critically Important Antibiotics, which is based on the degree of risk to human health due to resistance development following use in animals11.
Collaborative and cohesive initiatives taken by the farming sector, the veterinary profession and others in the food supply chain are demonstrating not only a serious commitment, but real progress in responding to the challenge of AMR. A One Health approach has shown that the health and welfare of people and animals is a priority for vets and farmers. The challenges faced are presenting real opportunities for the food and farming industry through the renewal of efforts to further enhance preventative animal health measures on farms and to sustainably deliver safe food for consumers.
Growing up on a beef farm in Ireland, GRACE O’GORMAN developed an early interest in animal health and a good understanding of the agri-food sector. After completing a degree in Biology and Masters in Biochemistry she embarked on a PhD at University College Dublin, where she had the opportunity to study parasitic disease in cattle and work at the International Livestock Research Institute (ILRI) in Kenya. After her PhD, Grace continued post-doctoral research on livestock, this time focusing on dairy cows. She complemented her scientific and research understanding of animal and veterinary public health with a degree in veterinary medicine. Grace has lectured on a range of animal health and welfare subjects, including One Health issues. She is currently a technical policy assistant at the National Office of Animal Health (NOAH), where she works on technical and communication aspects of various animal medicine topics.
References
- UK five year antimicrobial resistance strategy 2013 to 2018, P8 Section 2.1: www.gov.uk/…
- Farm Antibiotics – information on initiatives and work by the farming industry and others in the food producing supply chain to combat antibiotic resistance: www.farmantibiotics.org
- RCVS Code of Professional Conduct for Veterinary Surgeons: www.rcvs.org.uk/…
- NOAH briefing document: antibiotics for animal health and welfare, 2016: www.noah.co.uk/…
- Responsible Use of Medicines in Agriculture Alliance (RUMA): www.ruma.org.uk
- The UK Veterinary Medicines Regulations, 2013: www.legislation.gov.uk/uksi/2013/2033/contents
- European Medicines Agency (EMA) information on maximum residue limits: http://www.ema.europa.eu/…
- NOAH briefing document: controls on veterinary medicines, 2016: www.noah.co.uk/…
- VMD residues surveillance guidance: www.gov.uk/…
- RUMA press release, Dec 2016: Targets Task Force co-ordinates on antibiotic reduction in farming www.ruma.org.uk/…
- RUMA press release, May 2017: RUMA adopts European Medicines Agency ‘highest priority’ antibiotics list www.ruma.org.uk/…
Issue
Related topics
Food Safety, Health & Nutrition, Hygiene, Sustainability, The consumer
Related organisations
Noah, Responsible Use of Medicines in Agriculture Alliance (RUMA)







