The benefits of lower-protein infant and follow-on formula and the long-term impact on health
- Like
- Digg
- Del
- Tumblr
- VKontakte
- Buffer
- Love This
- Odnoklassniki
- Meneame
- Blogger
- Amazon
- Yahoo Mail
- Gmail
- AOL
- Newsvine
- HackerNews
- Evernote
- MySpace
- Mail.ru
- Viadeo
- Line
- Comments
- Yummly
- SMS
- Viber
- Telegram
- Subscribe
- Skype
- Facebook Messenger
- Kakao
- LiveJournal
- Yammer
- Edgar
- Fintel
- Mix
- Instapaper
- Copy Link
Posted: 29 April 2017 | Diana Salih - Nutrition Graduate at Nestle UK | No comments yet
With the global rise of obesity in children and adults and the subsequent impact on public health, early nutrition programming has become an area of growing interest1. One possible mechanism of such programming is the ‘early protein hypothesis’, proposing that a high protein intake during infancy and early childhood may increase the risk of adverse health outcomes, such as obesity, in later life2.


In response to the most recent science, the European Food Safety Authority (EFSA) has drafted a scientific opinion on the safety and suitability of follow-on formulas for infants over six months old with a protein content of approximately 1.1g/100ml (1.6g/100kcal). This is a lower level than that currently available in all follow-on milks in the UK and Ireland and a reduction from current regulations3. It is an example of the changes that have contributed to the evolution of infant and follow-on formulas over the years, lowering the protein content in an attempt to more closely mimic the composition of breast milk.
The protein content of mature breast milk is significantly lower than infant formula due to the high quality of the nutrition it provides4. This lower supply of protein from breast milk and the responsive nature of breastfeeding are some of the reasons why breastfed infants grow more slowly than bottle-fed infants. Breastfeeding is therefore regarded as a model of favourable programming as it’s associated with a lower obesity risk in school age and adolescence, compared with formula feeding5-9.
The importance of breastfeeding
As a global public health recommendation, infants should be exclusively breastfed for the first six months of life to achieve optimal growth, development and health10. The Department of Health supports this global recommendation and gives guidance to introduce solid foods at six months of age, along with the continuation of breastfeeding11. Breastfeeding is widely recognised as the ideal form of nutrition for infants, having unique advantages over bottle-feeding that extend beyond its role as a source of nutrition. Such advantages include supporting healthy growth and development; providing the infant with effective protection against infection and disease; and contributing to mother-infant bonding12.
Because the protein in breastmilk is adapted to a baby’s needs, a breastfed baby tends to grow more slowly than a formula fed baby13,14. This slower growth rate has shown significant long term health benefits including a lower risk of obesity, cardiovascular disease and diabetes15.
Although most mothers can successfully breastfeed, the majority of infants are fed formula by six months of age16. Manufacturers of infant formulas often add new ingredients in an attempt to more closely mimic the composition or outcomes of breast milk, aiming to produce a product that more closely replicates the advantages of breastfeeding3. In response to the growing evidence of the benefits of lower protein in breast milk compared to that of breast milk substitutes, some manufacturers are moving towards developing lower-protein formulas17.
The long-term impact of less protein in early infancy on latter health
Metabolic factors acting during critical windows of development can have lasting effects on health and disease risk in later life; this is known as ‘programming’18. The ‘early protein hypothesis’ represents a mechanism of programming whereby the observed benefit of the lower protein content in breast milk compared to infant formula, may reduce the risk of both early accelerated weight gain and later obesity8,19.
A proposed predictor of later obesity risk is accelerated weight gain during the first year of life20-24. Insulin-like growth factor (IGF-1) is a possible link between early protein intake and the increased risk of later obesity. Generally, circulating concentrations of insulin and IGF-1 are higher in formula-fed infants than in breastfed infants, which contributes to rapid growth in early infancy and thus increases their risk of adiposity23,25. The elevated concentrations of amino acids, which result from higher protein intake, may stimulate the secretion of insulin and IGF-1, which in turn increase cell proliferation and fat deposition, thereby contributing to early weight gain8,23,26.
Evidence therefore suggests that reducing the protein content of infant formulas may help to reduce early accelerated growth and early excessive weight gain6. In addition to later life obesity risk, there is convincing evidence that early life nutrition and consequent programming may be associated with other non-communicable diseases in later life, including type 2 diabetes, hypertension and cardiovascular disease27-31.
The history of protein improvements in infant formula
The development of infant formulas began at the start of the 20th century when it was known that the protein content of cows’ milk, on which infant formulas were based, was approximately three times higher than breast milk. In early formulas, the protein quantity was reduced but the quality, i.e. the amino acids that make up the protein structure, were not modified in any way32,33.


In early formulas, the protein quantity was reduced but the quality, ie the amino acids that make up the protein structure, were not modified in any way.
Based on the recognition that breast milk contains a higher proportion of whey-proteins, while cows’ milk is casein-dominant, formulas with a similar whey:casein ratio to breast milk were introduced in the 1960s3. Scientists were aware, however, that by increasing the proportion of whey protein the amount of minerals would increase with it. In 1961 the world’s first whey-dominant formula (60:40 whey:casein ratio) was created using an electrodialysis process that removed 95% of the minerals, allowing for a whey-dominant formula that did not have an unacceptably high renal solute load33.
In the 1990s research was directed towards lowering the protein content in infant formula while matching the amino acid profile of breast milk more closely34. In 2007 a new formula was marketed in the UK with a higher level of α-lactalbumin, a major protein component found in breast milk, containing increased levels of tryptophan and a balance of amino acids that resembled breast milk more closely than previous formulas. In 2009 a further improvement was made to this formula, reducing its protein content as supported with a clinical trial35.
Innovation in formula development has now resulted in lower-protein formulas with improved amino acid profiles that support slower growth in infants, which may be associated with long-term health benefits36. Further to the previous improvements in formula manufacturing, an original fractionation process of whey proteins has recently been developed that enables the removal of casein-glycomacropeptide (CGMP), a whey protein fraction that contains a high amount of threonine and low tryptophan37. In comparison with breast milk, the levels of the amino acid threonine in cows’ milk are higher, whereas tryptophan is lower and should therefore be modified38. The selective removal of CGMP from whey increases the α-lactalbumin proportion – a fraction very rich in tryptophan – resulting in an amino acid profile much closer to that of breast milk. This is characterised by comparable tryptophan and threonine levels and allows the adaptation of its protein content to resemble that of breast milk39.
Protein quantity and quality
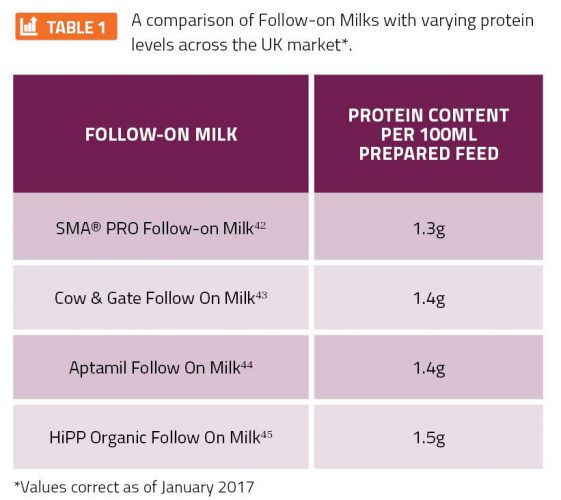
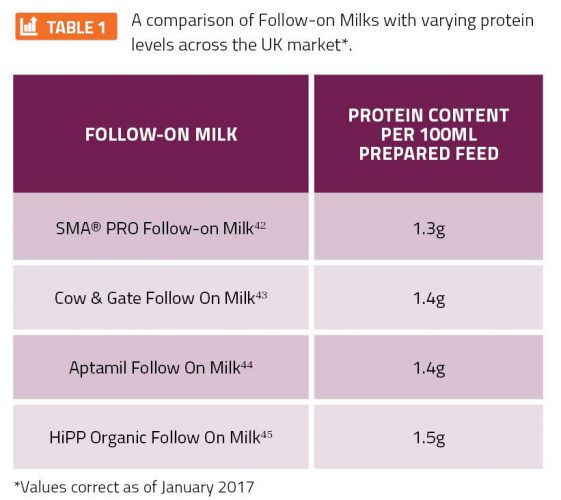
The development of infant and follow-on formula with optimised protein quality and quantity has been, and still is, the subject of focused investigation40. With the tendency in recent years for formula manufacturers to lower the protein content in an attempt to more closely mimic the growth of breastfed infants in that of formula-fed infants, there has been increased focus on the importance of reducing protein quantity whilst maintaining protein quality41. Varying methods of protein reduction in baby formula has ultimately resulted in significant differences in protein quantity and quality in the formulas available across the UK market (see Table 1, page 00).
The primary reason for the traditionally higher protein content of formula compared to that of breast milk was the lower digestibility of cows-milk protein, which limits the supply of essential amino acids. Therefore, when reducing the protein content of formula, it’s important for manufacturers to consider the impact that this may have on an infant’s blood serum concentrations of the essential amino acids, as this should not be lower than those in breastfed infants46.
Lowering the protein content in infant formula consequently results in a reduction of the amino acid tryptophan, of which high concentrations are found in breast milk47,48. One approach that has been used to avoid this limitation is to add free tryptophan to the formula49. Another approach is to increase the proportion of α-lactalbumin in formula as this protein has a high proportion of tryptophan, resulting in plasma tryptophan concentrations similar to those of breastfed infants50,51. The selective removal of CGMP, as previously discussed, is a new innovative method of altering the amino acid composition, which results in a superior quality protein and delivers an advantage over these other two methods52. The selective removal of CGMP results in a higher α-lactalbumin proportion, which increases tryptophan concentrations without the addition of tryptophan in the free form and results in an improved amino acid composition of the whey protein that is closer to that of breast milk.
The evidence
A multi-centre pooled analysis, published in September 2016, has resulted in conclusions that support the reduction of protein in infant formula. This study was conducted using individual participant data from 11 randomised controlled trials in six different countries. The primary objective was to assess the growth of infants fed a lower-protein infant formula and breastfed infants by comparing anthropometric z-scores with World Health Organization (WHO) growth standards. Conclusions were made that whey-predominant infant formula with a lower protein content (1.25g protein/100ml, lower than most currently available infant formulas) that more closely resembles breast milk, supports early growth comparable to the WHO growth standards and close to that of breastfed infants53. The selective removal of CGMP was used as the method of reducing the protein content in the lower-protein infant formula.
The evidence supporting the benefits of lower-protein formula and its impact on long-term health extend to long-term clinical trials. The European-wide Childhood Obesity Project (CHOP), set up in 2001 with a two-year follow-up, tested the hypothesis that a higher protein intake in infancy leads to more rapid length and weight gain in the first two years of life8. At the time of the two year follow-up, it was found that infants fed infant and follow-on formula with a lower-protein content for the first year of life had a significantly lower body mass index (BMI) compared to those fed higher-protein formula and were more similar to the group of breastfed infants54. A follow-up of this clinical trial at six years of age demonstrated that the infants fed a lower-protein infant formula had a lower BMI and obesity risk at school age6. Therefore, when combined, the evidence from these studies suggests that a lower protein intake in early childhood is likely to reduce the risk of obesity in later life, which supports the benefits of breastfeeding and lower-protein infant and follow-on formulas.
Conclusions
It is clear that breastfeeding is the best source of nutrition for infants with benefits extending to long-term health outcomes, such as the reduced risk of obesity. With this understanding, the innovation and reformulation of infant formula and follow-on milks aims to effect compositional changes, such as lower protein contents, that may result in a slower growth rate of formula-fed infants, comparable to that of a breastfed infant.
Historical innovation in infant and follow-on formula manufacturing have resulted in the reformulation of lower-protein formulas with amino acid profiles that more closely resemble that of breast milk. Recent clinical trials suggest that lowering the protein content of formulas further – to approximately 1.1g/100ml (1.6g/100kcal) – has proven to slow weight gain between three and six months of age and supports normal growth of infants after the age of three months20,55. With the emerging evidence and proposed changes in European recommendations from EFSA, it is likely that the future of infant and follow-on formula manufacturing will move towards the reformulation of even lower protein formulas.
About the author
Diana Salih is a Nutrition Graduate at Nestlé UK, working specifically in SMA Nutrition. Upon graduation, Diana took up a role as a Graduate at Nestlé UK with career aspirations to work in the food industry. Through her role in SMA Nutrition, Diana has worked on a number of projects within the Medical and Scientific Affairs team and has developed a specific scientific knowledge of infant nutrition.
References
- Koletzko, B., Brands, B., Poston, L. et al. (2012). Early nutrition programming of long-term health. Proceedings of the Nutrition Society. 71, 371-378.
- Gunther, A., Buyken, A. & Kroke, A. (2007). Protein intake during the period of complementary feeding and early childhood and the association with body mass index and percentage body fat at 7 y of age. American Journal of Clinical Nutrition. 85, 1626 – 1633.
- European Food Safety Authority (EFSA). (2017). Draft Scientific Opinion on the safety and suitability for use by infants of follow-on formulae with a protein content of at least 1.6g/100kcal. Available: https://www.efsa.europa.eu/sites/default/files/consultation/170113b.pdf. Accessed January 2017.
- Ballard, O. & Morrow, A. (2013). Human milk composition: nutrient and bioactive factors. Pediatr Clin North Am. 60(1), 49 – 74.
- Aaltonen, J., Ojala, T., Laitinen, K. et al. (2011). Impact of maternal diet during pregnancy and breastfeeding on infant metabolic programming: a prospective randomized controlled study. European Journal of Clinical Nutrition. 65, 10 – 19.
- Weber, M., Grote, V., Closa-Monasterolo, R. et al. (2014). Lower protein content in infant formula reduces BMI and obesity risk at school age: follow-up of a randomized control trial. The American Journal of Clinical Nutrition. 99, 1041 – 1051.
- Nestlé Nutrition Institute. (2013). Protein requirements in early childhood. Available: https://www.nestlenutrition-institute.org/News/Documents/7th%20NNI%20regional%20newsletter_Interactive%20(May2013).pdf. Accessed January 2017.
- Koletzko, B., Kries, R., Closa, R. et al. (2009). Lower protein in infant formula is associated with lower weight up to age 2 y: a randomized clinical trial. The American Journal of Clinical Nutrition. 89, 1836-1845.
- Harder, T., Bergmann, R., Kallischnigg, G. et al. (2005). Duration of breastfeeding and risk of overweight: a meta-analysis. American Journal of Epidemiology. 162(5), 397 – 403.
- World Health Organization. (2002). Infant and young child nutrition Global strategy on infant and young child feeding. Available: http://apps.who.int/gb/archive/pdf_files/WHA55/ea5515.pdf. Accessed: January 2017
- Department of Health. (2003). Infant Feeding Recommendations. Available: http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4096999.pdf. Accessed: January 2017.
- Horta, B. & Victoria, C. (2013). Long-term effects of breastfeeding: a systematic review. World Health Organization. Available: http://apps.who.int/iris/bitstream/10665/79198/1/9789241505307_eng.pdf. Accessed: January 2017.
- Lönnerdal, B. (2003). Nutritional and physiological significance of human milk proteins. The American Journal of Clinical Nutrition. 77, 1537-1543.
- WHO UK Growth Charts. Available: http://www.rcpch.ac.uk/child-health/research-projects/uk-who-growth-charts/uk-who-growth-chart-resources-0-4-years/uk-who-0. Accessed: January 2017.
- Singhal, A. & Lucas, A. (2004). Early origins of cardiovascular disease: is there a unifying hypothesis? 363, 1642 – 1645.
- Lennox, A., Sommerville, J., Ong, K. et al. (2013). Diet and nutrition survey of infants and young children. Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/139572/DNSIYC_UK_report_ALL_chapters_DH_V10.0.pdf. Accessed: January 2017.
- Hardwick, J. & Sidnell, A. Infant nutrition – diet between 6 and 24 months, implications for paediatric growth, overweight and obesity. Nutrition Bulletin. 39, 354 – 363.
- Koletzko, B., Dodds, P., Akerblom, H. & Ashwell, M. (2005). Early nutrition and its later consequences: new opportunities. New York: Springer Publishers.
- Owen, C., Martin, R., Whincup, P., Smith, G. & Cook, D. (2005). Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. 115, 1367 – 1377.
- Inostroza, J. Haschke, F., Steenhour, P., Grathwohl, D., Nelson, S. & Ziegler, E. (2014). Low-protein formula slows weight gain infants of overweight mothers. Journal of Pediatric Gastroenterology and Nutrition. 59(1), 70 – 77.
- Monteiro, P. & Victoria, C. (2005). Rapid growth in infancy and childhood and obesity in later life – a systematic review. Obesity Review. 6, 143 – 154.
- Ong, K. & Loos, R. (2006). Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta Paediatr. 95, 904 – 908.
- Kirchberg, F., Harder, U., Weber, M. et al. (2015). Dietary protein intake affects amino acid acylcarnitine metabolism in infants aged 6 months. J Clin Endocrinol Metab. 100(1), 149 – 158.
- Druet, C., Stettler, N., Sharp, S. et al. (2012). Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatr Perinat Epidemiol. 26, 19 – 26.
- Martin, R., Holly, J., Smith G. et al. (2005). Could associations between breastfeeding and insulin-like growth factors underlie associations of breastfeeding with adult chronic disease? The Avon Longitudinal Study of Parents and Children. Clin Endocrinol (Oxf). 62, 728 – 737.
- Koletzko, B., Kries, R., Monasterolo, R. et al. (2009). Can infant feeding choices modulate later obesity risk? The American Journal of Clinical Nutrition. 89, 1502S – 1508S.
- Koletzko, B., Brands, B. & Demmelmair, H. (2011). The EarlyNutrition Programming Project: five years of successful multi-disciplinary collaborative research. The American Journal of Clinical Nutrition. 94, 1749S – 1753S.
- Gluckman, P., Hanson, M. & Cooper, C. et al. (2008). Effect of in utero and early-life conditions of adult health and disease. New Engl J Med. 359, 61 – 73.
- Godfrey, K., Gluckman, P. & Hanson, M. (2010). Developmental origins of metabolic disease: life course and intergenerational perspectives. Trends Endocrin Met. 21, 199 – 205.
- Ruemmele, F. (2011). Early programming effects of nutrition – life-long consequences? Ann Nutr Metab. 58, 5 – 6.
- Koletzko, B. (2011). The power of programming: developmental origins of health and disease. Am J Clin Nutr. 94, 1747S – 2043S.
- Fomon, S. (2001). Infant feeding in the 20th Century: formula and beikost. The Journal of Nutrition. 131, 409S – 420S.
- Lien, E. (2003). Infant formulas with increased concentrations of α-lactalbumin. The American Journal of Clinical Nutrition. 77, 1555S – 1558S.
- Heine, W., Klein, P & Reeds, P. (1991). The importance of α-lactalbumin in infant nutrition. The Journal of Nutrition. 121, 277 – 283.
- Trabulsi, J., Capeding, R., Lebumfacil, J. et al. (2011). Effect of an α-lactalbumin-enriched infant formula with lower protein on growth. European Journal of Clinical Nutrition. 65, 167 – 174.
- Sidnell, A. & Greenstreet, E. (2009). Infant nutrition – protein and its influence on growth rate. Nutrition Bulletin. 34, 395 – 400.
- Räihä, N., Fazzolari-Nesci, A., Cajozzo, C. et al. (2002). Whey predominant, whey modified infant formula with protein/energy ratio of 1.8g/100kcal: adequate and safe for term infants from birth to four months. Journal of Pediatric Gastroenterology and Nutrition. 35, 275 – 281.
- Csapo, J. & Salamon, S. (2009). Composition of the mother’s milk. Protein contents, amino acid composition, biological value: a review. Acta Univ. Sapientiae, Alimentaria, 2(2), 174–195.
- Patent WO2004112508 A1. (2004). Infant or follow-on formula. Available: http://www.google.com/patents/WO2004112508A1?cl=en. Accessed January 2017.
- Macé, K., Steenhout, P., Klassen, P. & Donnet, A. (2006). Protein quality and quantity in cow’s milk-based formula for healthy term infants: past, present and future. Nestlé Nutrition Workshop, Pediatric Program. 58, 189 – 203.
- Fanaro, S. & Vigi, V. (2002). Protein quality and quantity in infant formulas. A critical look. Minerva Pediatr. 54(3), 203 – 209.
- SMA® PRO Follow On Milk datacard. Available: https://www.smahcp.co.uk/content/media/1561/sma-follow-on-data-card.pdf. Accessed January 2017.
- Cow & Gate Follow On Milk datacard. Available: https://www.eln.nutricia.co.uk/media/4335/datacard_cow__gate_follow_on.pdf. Accessed January 2017.
- Aptamil Follow On Milk datacard. Available: https://www.eln.nutricia.co.uk/media/4339/datacard_aptamil_follow_on.pdf. Accessed January 2017.
- HiPP baby milks comparison chart. Available: http://www.hipp4hcps.co.uk/Resources/Milks%20documents/13498-HIPP_HCP-Tick-Chart-25-Aug-2016-5th-PROOF.pdf. Accessed January 2017.
- Lönnerdal, B. (2014). Infant formula and infant nutrition: bioactive proteins of human milk and implications for composition of infant formulas. The American Journal of Clinical Nutrition. 99, 712S – 717S.
- Heine, W. (1999). The significance of tryptophan in infant nutrition. Adv Exp Med Biol. 467, 705 – 710.
- Lönnerdal, B. & Lien, E. (2003). Nutritional and physiologic significance of alpha-lactalbumin in infants. Nutr Rev. 61, 295 – 305.
- Fazzolari-Nesci, A., Domianello, D., Sotera, V. & Raiha, N. (1992). Tryotphan fortification of adapted formula increases plasma tryptophan concentrations to levels not different from those found in breast-fed infants. J Peditr Gastroenterol Nutr. 14, 456 – 459.
- Davis, A. Harris, B., Lien, E., Pramuk, K. & Trabulsi, J. (2008). Alpha-lactalbumin-rich infant formula fed to healthy term infants in a multicentre study: plasma essential amino acids and gastrointestinal tolerance. Eur J Clin Nutr. 62, 1294 – 1301.
- Sandström, O., Lönnerdal, B., Graverholt, G. & Hernell, O. (2008). Effects of alpha-lactalbumin-enriched formula containing different concentrations of glycomacropeptide on infant nutrition. Am J Clin Nutr. 87, 921 – 928.
- (European Patent: EP 0 880 902 A1.)
- Alexander, D., Yan, J., Bylsma, L. et al. (2016). Growth of infants consuming whey-predominant term infant formulas with a protein content of 1.8g/100kcal: a multicentre pooled analysis of individual participant data. The American Journal of Clinical Nutrition.
- De la Hunty, A. (2009). The EU Childhood Obesity Project. Nutrition Bulletin. 34, 403 – 406.
- Ziegler, E., Fields, D., Chernausek, S. et al. (2015). Adequacy of infant formula with protein content of 1.6g/100kcal for infants between 3 and 12 months. Journal of Pediatric Gastroenterology and Nutrition. 61(5), 596 – 603.
Issue
Related topics
Ingredients, Obesity, Proteins & alternative proteins, Research & development
Related organisations
European Food Safety Authority (EFSA), World Health Organization (WHO)